Are We Ready for the Next Pandemic?
A Retrospective on COVID-19 and the Search for Lessons to Combat Future Global Health Threats
In December 2019, the world witnessed the first genetically sequenced cases of COVID-19 emerging from Wuhan, China.
Although some studies suggest that the SARS-CoV-2 virus may have infected humans before December 2019, these claims rely on indirect methods like the presence of antibodies in stored blood samples, which remain inconclusive.
The World Health Organization (WHO) hesitated to label the crisis a 'pandemic' until March 11, 2020, by which time over 100,000 confirmed cases had spread across more than 100 countries, resulting in at least 4,000 deaths globally.
Shortly after, on March 19, 2020, Serbia declared an epidemic as the virus had infected 118 people with the first confirmed case recorded in Bačka Topola on March 6.
Globally, COVID-19 eventually infected a large portion of the population, claiming the lives of at least 15 million people and leaving over 400 million with long-term health issues.
Though the mortality rate of COVID-19 was moderate, experts warn that future pandemics could potentially be more severe.
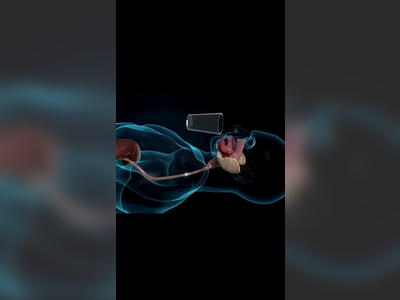
Such global health threats commonly arise from airborne respiratory viruses that spread through sneezing, coughing, speaking, and singing.
Despite this, during the early months of the pandemic, WHO experts insisted that coronavirus was not airborne, recommending hygiene practices like social distancing and regular handwashing as the primary protective measures.
MASS MANDATES AND PUBLIC PERCEPTION
Early in the pandemic, mask-wearing was advised by WHO only as a precautionary measure, despite its known efficacy in preventing air-transmitted diseases like influenza and tuberculosis.
Nevertheless, as the pandemic evolved and the Omicron variant became prevalent, the WHO incorporated mask-wearing and room ventilation into its recommendations.
According to a Science magazine article by Lydia Morawska from Queensland University of Technology, the WHO began using the term 'airborne transmission' more prominently.
The potential spread of avian influenza H5N1, currently transmitted among wild birds and able to infect humans, raises concerns.
To cause a pandemic, such animal-origin viruses would need to spread easily from person to person, a capability they traditionally lack.
However, viruses constantly acquire mutations and can exchange genes through recombination, creating new strains potentially capable of efficient human-to-human transmission.
The 1918 Spanish flu pandemic, which killed an estimated 40 to 50 million people, exemplifies the devastating impact of a virulent recombined virus.
More researchers today argue that pandemic risk is increasing as human populations encroach on new habitats, exposing individuals to novel viruses.
Climate change-induced animal migrations and the growing number of domestic livestock further contribute to this risk, as seen with dangerous mutations of H5N1 arising from duck farms in China.
Meanwhile, global travel facilitates the rapid international spread of emerging epidemics.
SIGNIFICANCE OF LABORATORY SECURITY
Though no direct evidence links the origin of SARS-CoV-2 to laboratory escape, past incidents, like the 1977 influenza outbreak in the Soviet Union, suggest such risks are plausible.
This particular outbreak may have originated from a virus strain accidentally released from long-term lab storage.
While the probability of such events remains low, the potential severity—imagine an inadvertently released virus resulting in mass casualties—demands vigilant concern.
Research inevitably involves risks, yet its potential benefits can outweigh these dangers.
Stringent regulations have been enforced globally for viral experimentation, yet accidents could occur in any location.
Virginie Courtier of the French National Centre for Scientific Research advocates for tighter controls and cautions against publishing high-risk findings in leading scientific journals.
Rather than solely searching for new animal viruses, Virginie Courtier suggests resource allocation towards identifying viruses already infecting humans.
Such efforts could preemptively curb potential pandemics, akin to the successful containment of the SARS outbreak originating in China in 2003.
Maintaining an infrastructure capable of swift virus detection and response is imperative, although current capabilities fall short.
Promising innovations, such as wastewater surveillance for pathogen detection, face cost prohibitions on the global scale.
Emphasis, therefore, should be placed on expediting the development of diagnostics, treatments, and vaccines to address hypothetical pandemics.
TRUST AND COMMUNICATION
Research from the Coalition for Epidemic Preparedness Innovations (CEPI) indicates that 60% of epidemiologists believe we are now better prepared for future pandemics.
Yet issues in public trust and the dissemination of misinformation remain a primary concern.
Despite vaccines saving millions during the COVID-19 pandemic, they failed to halt its spread entirely, highlighting the need for vaccines that both reduce transmission and the severity of infections.
Researchers acknowledge the unpredictable nature of public behavior during crises, stressing that victory over viruses involves not just scientific advancements but also public confidence in medicine and science.
In the event of a future pandemic, adherence to health guidance and acceptance of vaccination will be crucial determinants of global response efficacy.
Although some studies suggest that the SARS-CoV-2 virus may have infected humans before December 2019, these claims rely on indirect methods like the presence of antibodies in stored blood samples, which remain inconclusive.
The World Health Organization (WHO) hesitated to label the crisis a 'pandemic' until March 11, 2020, by which time over 100,000 confirmed cases had spread across more than 100 countries, resulting in at least 4,000 deaths globally.
Shortly after, on March 19, 2020, Serbia declared an epidemic as the virus had infected 118 people with the first confirmed case recorded in Bačka Topola on March 6.
Globally, COVID-19 eventually infected a large portion of the population, claiming the lives of at least 15 million people and leaving over 400 million with long-term health issues.
Though the mortality rate of COVID-19 was moderate, experts warn that future pandemics could potentially be more severe.
Such global health threats commonly arise from airborne respiratory viruses that spread through sneezing, coughing, speaking, and singing.
Despite this, during the early months of the pandemic, WHO experts insisted that coronavirus was not airborne, recommending hygiene practices like social distancing and regular handwashing as the primary protective measures.
MASS MANDATES AND PUBLIC PERCEPTION
Early in the pandemic, mask-wearing was advised by WHO only as a precautionary measure, despite its known efficacy in preventing air-transmitted diseases like influenza and tuberculosis.
Nevertheless, as the pandemic evolved and the Omicron variant became prevalent, the WHO incorporated mask-wearing and room ventilation into its recommendations.
According to a Science magazine article by Lydia Morawska from Queensland University of Technology, the WHO began using the term 'airborne transmission' more prominently.
The potential spread of avian influenza H5N1, currently transmitted among wild birds and able to infect humans, raises concerns.
To cause a pandemic, such animal-origin viruses would need to spread easily from person to person, a capability they traditionally lack.
However, viruses constantly acquire mutations and can exchange genes through recombination, creating new strains potentially capable of efficient human-to-human transmission.
The 1918 Spanish flu pandemic, which killed an estimated 40 to 50 million people, exemplifies the devastating impact of a virulent recombined virus.
More researchers today argue that pandemic risk is increasing as human populations encroach on new habitats, exposing individuals to novel viruses.
Climate change-induced animal migrations and the growing number of domestic livestock further contribute to this risk, as seen with dangerous mutations of H5N1 arising from duck farms in China.
Meanwhile, global travel facilitates the rapid international spread of emerging epidemics.
SIGNIFICANCE OF LABORATORY SECURITY
Though no direct evidence links the origin of SARS-CoV-2 to laboratory escape, past incidents, like the 1977 influenza outbreak in the Soviet Union, suggest such risks are plausible.
This particular outbreak may have originated from a virus strain accidentally released from long-term lab storage.
While the probability of such events remains low, the potential severity—imagine an inadvertently released virus resulting in mass casualties—demands vigilant concern.
Research inevitably involves risks, yet its potential benefits can outweigh these dangers.
Stringent regulations have been enforced globally for viral experimentation, yet accidents could occur in any location.
Virginie Courtier of the French National Centre for Scientific Research advocates for tighter controls and cautions against publishing high-risk findings in leading scientific journals.
Rather than solely searching for new animal viruses, Virginie Courtier suggests resource allocation towards identifying viruses already infecting humans.
Such efforts could preemptively curb potential pandemics, akin to the successful containment of the SARS outbreak originating in China in 2003.
Maintaining an infrastructure capable of swift virus detection and response is imperative, although current capabilities fall short.
Promising innovations, such as wastewater surveillance for pathogen detection, face cost prohibitions on the global scale.
Emphasis, therefore, should be placed on expediting the development of diagnostics, treatments, and vaccines to address hypothetical pandemics.
TRUST AND COMMUNICATION
Research from the Coalition for Epidemic Preparedness Innovations (CEPI) indicates that 60% of epidemiologists believe we are now better prepared for future pandemics.
Yet issues in public trust and the dissemination of misinformation remain a primary concern.
Despite vaccines saving millions during the COVID-19 pandemic, they failed to halt its spread entirely, highlighting the need for vaccines that both reduce transmission and the severity of infections.
Researchers acknowledge the unpredictable nature of public behavior during crises, stressing that victory over viruses involves not just scientific advancements but also public confidence in medicine and science.
In the event of a future pandemic, adherence to health guidance and acceptance of vaccination will be crucial determinants of global response efficacy.
AI Disclaimer: An advanced artificial intelligence (AI) system generated the content of this page on its own. This innovative technology conducts extensive research from a variety of reliable sources, performs rigorous fact-checking and verification, cleans up and balances biased or manipulated content, and presents a minimal factual summary that is just enough yet essential for you to function as an informed and educated citizen. Please keep in mind, however, that this system is an evolving technology, and as a result, the article may contain accidental inaccuracies or errors. We urge you to help us improve our site by reporting any inaccuracies you find using the "Contact Us" link at the bottom of this page. Your helpful feedback helps us improve our system and deliver more precise content. When you find an article of interest here, please look for the full and extensive coverage of this topic in traditional news sources, as they are written by professional journalists that we try to support, not replace. We appreciate your understanding and assistance.